冠状动脉造影术评估人工智能,用于动脉粥样硬化的个性化医学治疗:QCI研究组的共识陈述
作者:Dewey, Marc
介绍
冠状动脉血管造影(CCTA)已成为可疑冠状动脉疾病(CAD)患者的一线成像方式,仅在欧洲,每年在欧洲就进行220万种CCTA手术1,,,,2,,,,3,,,,4。将CCTA作为稳定CAD中间概率的患者进行CCTA作为第一道研究5,,,,6由关键的随机,受控的心血管结局试验支持,例如Scot-Heart3和排放7,,,,8试验。这些研究表明,CCTA比标准护理和侵入性冠状动脉造影在减少主要不良心血管事件(MACE)方面的优势和CCTA与侵入性冠状动脉血管造影的不介绍性在减少与主要程序相关的主要并发症方面具有优势。在苏格兰人的审判中7,在标准护理中添加CCTA降低了主要结局指标的发生率(MACE;冠心病相关的死亡和非致命性心肌梗死),最初的5年研究期以及最多10年的延长随访期9。这些发现主要归因于提高的诊断精度和优化的预防疗法10并与将侵入性治疗与准确风险预测联系起来的手术文献的证据一致11,,,,12。同样,出院试验8,,,,13结果表明,CCTA是胸痛稳定且CAD中进行中间测试概率的患者的初始诊断策略,导致MACE的发生率(心血管死亡,非致命性心肌梗塞或非致命性中风;主要结果),与无形的冠状血管造影(HR 0.70.70,95%CI)相似。就继发性结果而言,CCTA的使用与主要程序相关并发症的发生率较低(HR 0.26,95%CI 0.13 0.55),尤其是在女性中(HR 0.14,95%CI 0.04-0.04 - 0.46)14在<65岁的患者中(OR 0.10,95%CI 0.02-0.36)15。来自临床试验的证据导致了CCTA的全球采用,并随后不断发展的记录政策。除了检测阻塞性CAD之外,CCTA还可以定量冠状动脉粥样硬化
6,,,,16为动脉粥样硬化斑块负担提供关键的见解。但是,此量化的可靠性仍然可变17尽管临床使用越来越多,但它是成功实施CCTA的临床实施的阿基里斯的脚跟18。人工智能(AI)和机器学习的进步(ML)现在可以随着速度和可靠性提高而详细的量化和特征19。但是,将这些技术进步转化为临床实践的挑战仍然存在。需要为每个CCTA发现指定临床治疗建议的明确,基于证据的指导,尤其是对于胸痛稳定和CAD中间可能性的患者,在其中证明了CCTA的临床价值。这份通过Delphi流程制定的专家共识声明解决了这些挑战,并提供了将CCTA和AI工具纳入心血管护理中的循证建议。通过将成像技术中的创新与量身定制的治疗策略联系起来,我们旨在优化结果并减轻动脉粥样硬化CAD的全球负担。
AI支持工具的潜力
AI支持的工具(通常包含机器学习技术)有望改变医疗图像分析,提供改善患者护理和加速科学发现的机会20,,,,21,,,,22。评估动脉粥样硬化斑块的AI支持工具是可靠且快速的,使临床医生和研究人员能够提高效率和精度23。大多数用于动脉粥样硬化斑块分析的自动化工具和服务首先识别和标记CCTA上的冠状动脉分支24,分段冠状动脉和外容器边界,最后对动脉粥样硬化斑块进行亚分析,通常基于测量的衰减值25或高级深度学习支持的动脉粥样硬化斑块表征的方法26。尽管使用CCTA成像小型移动结构的技术挑战,但已证明了AI支持的动脉粥样硬化斑块定量和血管内超声检查(IVU)之间的高精度和一致性。27,,,,28。然而,迄今为止,还没有进行过大规模的,动脉粥样硬化的斑块分析工具和服务之间的面对面比较。
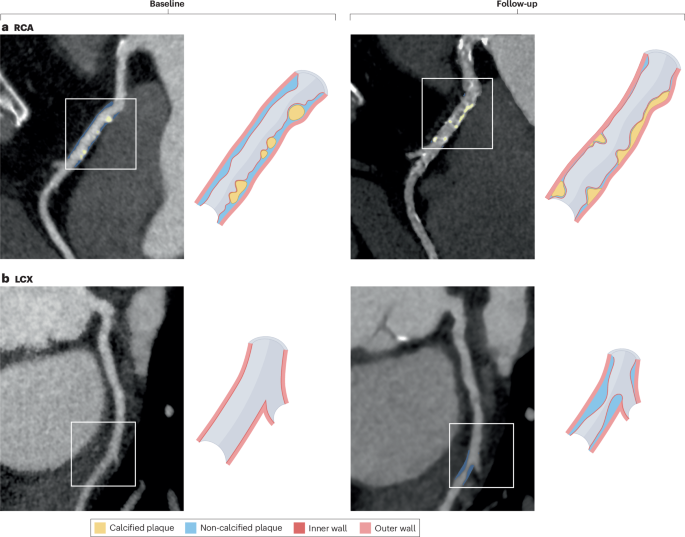
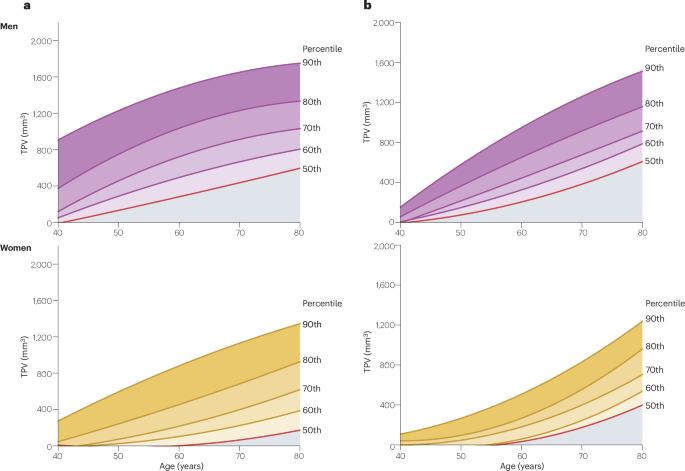
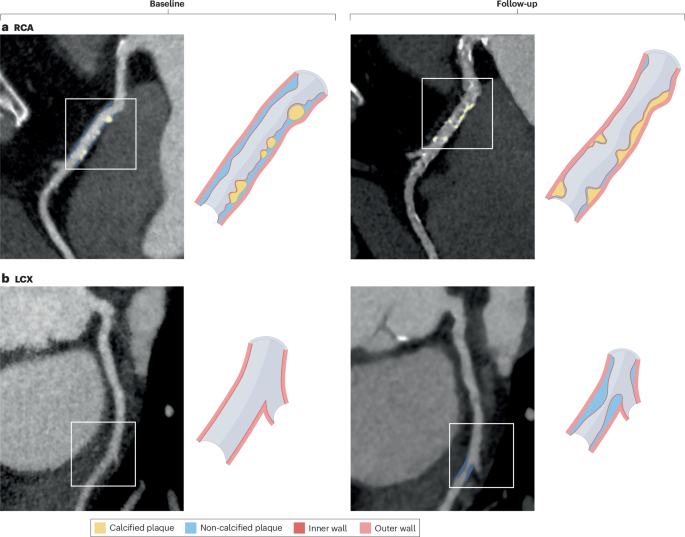
原则上,对CCTA上的冠状动脉粥样硬化的AI支撑分析允许对年龄调整和性别调整的百分位曲线产生用于动脉粥样硬化成像生物标志物的,例如冠状动脉成像,例如冠状动脉总斑块量(TPV)29。这种方法为个性化的风险分层和基于成像的治疗提供了潜力。一种特殊的应用是在患有稳定的胸痛和可疑CAD的患者中启动降低脂质和抗动脉粥样硬化剂的阈值,但没有I级的汀类药物疗法。AI支持的CCTA(仿生放射科医生)对人的CCTA分析可能会导致更大的可靠性和更具成本效益的动脉粥样硬化成像30。此外,识别动脉粥样硬化斑块的不良特征可以实现个性化的管理策略31。有趣的是,可以通过监测随访过程中的动脉粥样硬化斑块的变化来衡量对治疗的反应(图 1)。这种方法已用于各种大规模,正在进行的研究项目中,但尚未包含在临床实践指南中。AI支持的工具的进步对研究具有进一步的影响。在相当短的时间范围内分析大型图像的大型图像的能力有助于病理生理,药理和技术发现,并可以提高我们对治疗效果的理解32。由于AI支持的动脉粥样硬化斑块量化和IVUS之间的高度一致性,因此对冠状动脉粥样硬化变化的无创测量也有可能扩大CCTA在临床研究中的作用。33,,,,34。在此共识声明的后面,详细讨论了AI支持的动脉粥样硬化成像的应用,局限性和可靠性。
范式转移
预防和治疗冠状动脉粥样硬化包括几种策略,包括作为独立方法的靶标(LDL胆固醇(LDL-C)降低),或者是基于综合风险因素的策略的一部分35,,,,36。一个包括干预和最少随访的火灾模型在全球临床实践中也很普遍。尽管这些常规的预防和治疗方法导致了CAD年龄标准化死亡率的全球降低,但冠状动脉粥样硬化的患病率上升和持续的区域差异,它们的局限性得到了强调37,,,,38。
Treat-to-toget模型虽然有效地实现了指南示意的LDL-C水平,但通常无法解决残留的心血管风险39。这种方法的关键局限性是动脉粥样硬化斑块负担和形态不被考虑40这两个对于准确个性化心血管风险评估至关重要41。动脉瘤负担使用高级技术来对冠状动脉进行成像,与LDL-C的浓度不一致,并且在当前的管理策略框架中仍未发现32。同样,基于风险因素的策略通常过度简化了患者和动脉粥样硬化斑块的异质性和脆弱性,从而忽略了共存的病理生理机制的相互作用。尽管从理论上讲是全面的,但这些方法可能无法识别出最小的传统危险因素但具有冠状动脉粥样硬化的高风险个体,而过度治疗的其他人患有危险因素但没有冠状动脉粥样硬化的动脉粥样硬化42,,,,43。众所周知,临床风险因素估计值是动脉粥样硬化负担的较差预测指标,而基于CCTA的动脉粥样硬化斑块的定量已显示为长期结局具有较高的预测值44。
历史上提出的火灾方法是一种基于人群的管理策略,主要用于初级预防,也可能导致过度治疗或不足,潜在地增加不良影响或使动脉粥样硬化斑块均无所足45。此外,涉及固定剂量疗法的方法,没有随后的患者监测或合并症治疗不足,无法适应患者特征的变化或动脉粥样硬化的动态自然病史。为了克服这些局限性,我们提出了一个范式转移,强调了由CCTA衍生的,AI支持的动脉粥样硬化斑块评估的个性化治疗建议的整合(图。 2)。这种方法使用基于百分位的风险分层和患者量身定制的治疗方法,将当前策略的优势结合在一起,同时减轻其弱点。
冠状动脉疾病的常规治疗策略包括治疗(调整疗法以实现特定目标),基于风险因素的治疗(专注于通过解决多个危险因素来管理总体心血管风险)和火灾或遭受遗嘱(开处方固定剂量的药物而无需监测特定目标的情况下)。这些策略通常忽略了病理的复杂性,而忽略了个性化疗法的益处。人工智能(AI)对动脉粥样硬化斑块的评估可以通过揭示每个患者中疾病调节冠状动脉粥样硬化的程度和性质,并通过基于年龄调整和性别调整的冠状冠状动脉冠状动脉量(TPV)含量(TPV)百分位来改善患者管理。所描述的百分位曲线仅用于说明目的,不代表实际数据。根据定量心血管成像研究小组第三次会议后进行的Delphi共识过程,如果检测到任何冠状动脉粥样硬化斑块的存在,并将治疗升级升级到高强度方案(桌子)(桌子)(桌子)(桌子)(桌子)(表)(桌子)(表)(桌子)(表)(桌子) 1当在冠状动脉血管造影上达到第70%的TPV阈值时,建议)。
生成共识建议的方法
基于AI支持的动脉粥样硬化斑块的人群分布的人群百分位数,需要从众多领域提出明确的治疗建议。因此,我们组装了35名专家的定量心血管成像(QCI)研究小组,包括12位心脏病专家,11位放射科医生,5位计算机科学家,3位生物医学工程师和科学家,2名全科医生,1名射线照相师和1名流行病学家。专家谈判是在2024年9月6日在德国柏林市的第三届QCI研究小组共识会议上举行的。与我们以前的共识流程相似6,,,,20,,,,46,我们使用Delphi方法生成并询问参与者一组12个问题(补充材料 1)总共三轮。该问卷旨在提出有关将CCTA上的动脉粥样硬化斑块成像转换为医疗建议的可行性和最佳方法的专家意见。我们评估了四个关键点:动脉粥样硬化斑块测量的可靠性,用于治疗起始和升级的动脉粥样硬化斑块表型的有意义,将动脉粥样硬化斑块分析的转换转化为明确的医疗治疗建议以及对治疗建议升级的风险调节剂。我们包括各种类型的问题,包括二进制问题,排名问题和定量问题(补充材料 2
)。5点李克特量表主要用于定量问题,但是当需要在五个以上的类别上进行比较时,使用9分制来捕获专家意见的更细微的区别。第一次Delphi回合发生在第三次QCI学习小组共识会议之后2周。
参与者通过Welphi Web应用程序收到了与问卷的个性化和匿名链接。第二轮和第三轮比赛在上一轮后1周开始。该过程旨在促进专家意见的交流和融合,以获得对讨论的主题的集体理解,理想情况下,以简化且一致的方式达成共识。为了实现这一目标,在第二轮和第三轮问题中,参与者从上一轮的在线工具中向参与者展示了他们的答案,并在被认为适当的情况下可以修改他们。此外,在第二轮和第三轮比赛中,所有专家在上一轮问题中给出的匿名临时答复被显示为框图和条形图。在问卷中提供了有关多个问题的相关信息,包括当前的文献以及从苏格兰人和出院试验的数据分析得出的证据和未发表的证据29(补充材料 3)。QCI研究小组的共识建议总结在盒子中 1。
在本文中讨论的许多试验中,参与者根据问卷而自行报告为“女性”或其他,而没有进一步澄清生物学性别。鉴于这些信息是作为自我报告的身份而不是生物学分类收集的,因此我们选择使用“性别而不是性别”一词,以与原始数据保持一致。
个性化治疗建议的生物标志物和临床参数
冠状动脉粥样硬化斑块
在临床实践中,CCTA通常用于区分钙化和非鉴定斑块(NCP)成分。每种动脉粥样硬化斑块表型都有不同的临床适应症,使其非常适合定义治疗建议(Box” 2)。可用的证据表明,动脉粥样硬化始于内皮功能障碍,导致内皮对LDL的渗透性增加。随后的炎症反应吸引了巨噬细胞,可渗入内膜并吞噬氧化的LDL形成泡沫细胞,从而扩大炎症并刺激平滑肌细胞的增殖。动脉粥样硬化斑块的进展继续随着富含脂质的坏死核和纤维帽的发展而持续。一些动脉粥样硬化斑块钙化,钙沉积很大,导致稳定性,而另一些则由于纤维帽和持续的炎症而易受伤害47,,,,48。
钙化斑块
冠状动脉钙(CAC)评分广泛用于风险分层,尤其是无症状患者的一级预防。在有症状的患者中,CAC还显示出基于风险因素的评估以外的预后相关性49。CCTA评估的CAC评分和钙化斑块体积(CPV)的预后效用已在许多观察性研究中得到证明49,,,,50,,,,51,,,,52,,,,53,,,,54,,,,55,,,,56,,,,57。此外,Eisner研究58证明,使用CAC评分的共同决策对2137例无症状的患者组成的人群中对生活方式的改变和医疗建议的依从性有积极影响,他们的预测概率较低。值得注意的是,CAC评分的高阴性预测值可以排除广泛的动脉粥样硬化CAD,并易于执行,低风险和低成本成像。
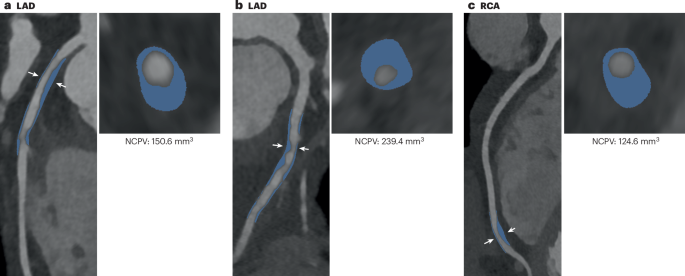
尽管其预后相关性,但使用CAC评分或CPV提出治疗建议仍受到多种因素的限制。首先,尽管几项研究表明CAC得分与MACE之间存在很强的关联,但尚未证明直接的因果关系。易受伤害的动脉粥样硬化斑块容易破裂,主要由炎症NCP组成32,而在每个患者和每个子宫基础上,密集钙化的动脉粥样硬化斑块的比例与动脉粥样硬化CAD事件的风险成反比59。其次,CAC评分和CPV与年龄密切相关,并且使用这些措施预测动脉粥样硬化的CAD事件可能会高估风险,尤其是在老年人中。相反,专注于CPV(或CAC得分)作为预测因子可能会导致CPV低和NCP量较高(NCPV)的风险低估,尤其是在年轻人中(图。 3)狼牙棒(在动脉粥样硬化的多种族研究中,在事件之前的成像中有25%的成像得分为0)60,,,,61。第三,在降低脂质疗法的动脉粥样硬化斑块稳定后,CAC评分和CPV增加,而MACE的风险降低62。由于降低脂质药物的广泛处方,CAC评分或CPV和MACE之间的相关性很模糊63。因此,CAC评分或CPV不是治疗功效纵向评估的首选标记。总体而言,数据表明,尽管证明在一般人口水平上具有预后,但CAC评分和CPV对于确定个体治疗建议的适用性有限。然而,使用CPV和NCPV或总斑块负担进行预测之间的研究数量是有限的,需要进一步的随机研究。
非倒数牌匾
NCP是冠状动脉粥样硬化斑块的重要组成部分,该斑块无法在非对比度CT上可视化。在CCTA上,可以将NCP识别为NCPV,也可以归一化为血管或段的体积或面积。NCP结合了包括各种亚型的一系列衰减值,包括纤维,纤维曲霉和低衰减NCP。在发育的早期阶段,动脉粥样硬化斑块通常是未估计的;它们可以代表代谢活性的CAD,特别是在存在低衰减斑块的情况下,或者可能表示较老的纤维化疾病。由于这种病理生理学,年轻患者的NCP量往往比钙化的动脉粥样硬化斑块大。随着时间的流逝,NCP可以进展和钙化,从而表明通过增加CPV和NCPV减少或保持稳定而对治疗的反应。NCPV是一个有价值的预后标记,与视觉和定量评估中Maces的风险增加有关32,,,,64。在对苏格兰人试验的回顾性分析中32在1,769例胸痛稳定的患者中,低触发NCP负担是5年后的致命或非致命性心肌梗死的最强预测指标(调整后的HR 1.60,95%CI 1.10 1.10 2.10 2.10 2.34每增加一倍的动脉粥样硬化斑块负担)。在Rapid-CTCA试验中对422名患者的事后评估中65,TPV(HR 25.4,95%CI 3.44 188.0),NCPV(HR 26.4,95%CI 3.58 – 196.0)和低衰减动脉粥样硬化斑块(HR 7.80,95%CI 2.33 26.0)是未来的非法律效果的强烈预测者,是未来的非法律效果。此外,NCPV可用于评估新的医疗疗法作为MACES之前几年的替代成像终点66。例如,蒸发试验的主要结果分析37在68例甘油三酸酯水平升高的患者中,用ICOSAPENT乙基治疗18个月后,低衰减NCPV的降低降低降低,并进行了缓刑试验的回顾症33,,,,67结果表明,pitavastatin疗法导致611例HIV患者和未知心血管疾病(CVD)的NCPV降低。
尽管测量NCPV在冠状动脉成像中具有优势,但并非所有患者都有NCP。在迈阿密心脏研究队列中(n= 2,459),观察到近50%的患有动脉粥样硬化斑块的参与者仅具有钙化的斑块,强调了种群中斑块组成的异质性68。因此,NCPV的作用尚不清楚。QCI研究小组对NCPV本身的使用达成了共识。但是,无论是作为风险调节剂(57%的选票),作为TPV(40%票数的40%)还是仅使用TPV(3%的选票)(补充材料)(补充材料) 1)。如果被证明是可操作的成像生物标志物,NCPV将来可能有助于指导患者管理,并且可能是最适合监视治疗反应的标记。
总牌匾
CCTA通过提供CAD的详细证据来有效地识别并分层心肌梗塞的未来风险。缺乏动脉粥样硬化疾病与极低的MAS(每1000名患者年少于一个心肌梗死)有关69。从历史上看,CAD的风险分层一直集中在阻塞性疾病的存在上,伴有预后价值的狭窄的数量和严重程度。但是,大多数心肌梗死是由非刺激性疾病引起的,部分原因是普通人群中非刺激性疾病的患病率更高。几项基于CT的临床试验表明,在随后发生心肌梗死的发生中,非刺激性疾病的主导地位,以及大多数患有心肌梗塞的人都没有证据表明在功能胁迫测试上缺血的事实70,,,,71。这些发现导致了以下假设:TPV是风险分层最重要的指标。确实,狭窄疾病的程度比仅仅是疾病的存在更重要,并且是风险的非常有力的预测指标69。TPV结合了CPV和NCPV,使用AI支持的分析是临床实践中最可靠的成像生物标志物25,,,,72,,,,73。QCI研究小组认为TPV是启动或升级医疗建议的最有意义的参数(图。 4)。此外,可以使用AI工具可靠地评估TPV,并对临床试验人群中的MAS具有预后价值74。但是,与CPV相似,TPV不适合监测药物反应,因为此措施没有区分NCPV和CPV的变化,这是风险评估所必需的。
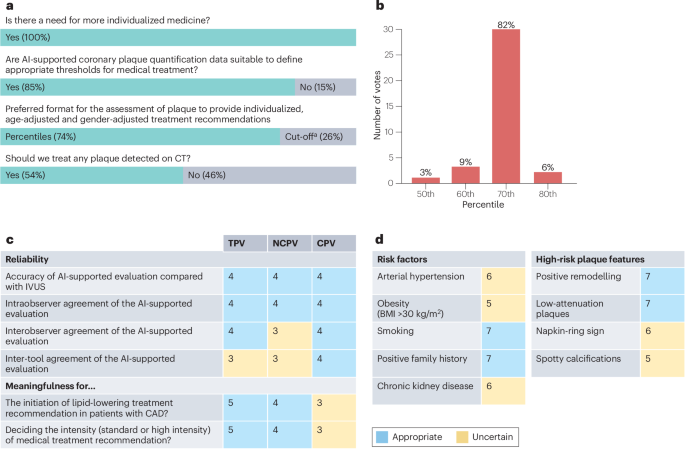
在基于人工智能(AI)支持的动脉粥样硬化斑块量化基于人工智能(AI)的个性化医疗方面,显示了35名专家(定量心血管成像研究组)的关键建议。一个,有关冠状动脉粥样硬化斑块的适用性和首选措施的问题,以指导治疗建议。b,对适当的年龄调整和性别调整的百分位数阈值(TPV)的投票结果,用于启动高强度降低脂质的治疗。当TPV高于第70个百分位时,专家组就升级为高强度方案达成共识(82%)。c在5点Likert量表上,对AI支持的TPV定量,非鉴定的斑块体积(NCPV)和钙化的斑块体积(CPV)的可靠性和有意义,以5点Likert量表(1â2â= - 不合适,3 =不确定),4-5 = - 适用)。d,在存在9点李克特量表的危险因素或高风险斑块特征的情况下,医疗治疗升级的适当性(1 3 =不合适,4â=不确定,不确定,7 9 =合适)。没有动脉粥样硬化斑块措施或风险调节剂不合适。面板中的值c和d是中位数。一个动脉粥样硬化斑块体积的数值截止值。BMI,体重指数;CAD,冠状动脉疾病;IVU,血管内超声检查。
高风险牌匾特征
在研究了动脉粥样硬化斑块的各种半定量特征中,有四个证明了预后的相关性,并被统称为高风险斑块特征6,,,,25,,,,75:低衰减牌匾,餐巾纸标志,阳性重塑和斑点钙化18,,,,76。在苏格兰人的审判中32,低衰减斑块负担是对心肌梗塞未来风险的最强预测指标。此外,稳定CAD患者的荟萃分析确定餐巾纸标志是预测MACES的最强高风险牌匾特征(HR 5.06,95%CI 3.23 7.94)76。几项研究表明,急性冠状动脉综合征患者的重塑指数比稳定CAD患者更高77,,,,78,,,,79。尽管具有广泛钙化的动脉粥样硬化斑块通常在临床上保持沉默,但急性冠状动脉综合征的加速疾病进展和罪魁祸首是斑点的钙化80,,,,81。在CCTA定义的高风险牌匾特征中,出现了低衰减斑块和阳性重塑作为评估心血管风险的最重要特征82。
动脉粥样硬化斑块中的CT衰减测量受到诸如腔内对比度浓度,管电压,切片厚度和重建过滤器等因素的影响83,,,,84,,,,85,,,,86。此外,在日常练习中,高风险的斑块特征在很大程度上被报道为视觉措施87,,,,88。图像质量,读取器体验和软件的差异会影响动脉粥样硬化斑块的一致性89。这种情况导致了中等观察者的一致性,以识别高风险牌匾特征,并具有κ在研究环境中的值范围为0.56至0.6990,,,,91。此外,来自光子计数CT的不同虚拟单核图像改变了衰减值,因此,相应的动脉粥样硬化斑块特征进一步有助于降低可重复性92。
尽管高风险的牌匾特征表现出强大的总体预测性能,但由于三个原因,它们并不适合确定治疗建议。首先,它们的积极预测价值低,大多数具有此类特征的患者都不会发生事件。Second, high-risk plaque features are not present in all patients with atherosclerotic plaque and, therefore, patients without such features who might benefit from treatment would be missed.Third, the reliability of assessing high-risk plaque features is limited.However, high-risk plaque features could inform the adjustment of existing treatment, such as escalating dose intensity.Further investigation and improvements are needed to improve reproducibility and interobserver agreement in assessing high-risk plaque features93。
Additional risk modulators
Cardiovascular risk factors, such as smoking, obesity and a family history of CVD, have been well defined for many years and can be directly linked to an increase in the rate of CVD progression.Shifting the focus of treatment from LDL-C to plaque-based recommendations does not diminish the importance of risk factors.Their integration as factors that modulate treatment intensity is crucial to the individualization of patient management.
Non-modifiable and modifiable risk factors
Assessment of cardiovascular risk using validated scoring systems, such as the Systematic Coronary Risk Evaluation (SCORE), SCORE2 and atherosclerotic CVD (ASCVD) 2013 Risk Calculator, is a fundamental component of the clinical decision trees recommended by major international guidelines to inform the use of preventative therapies94,,,,95。In general, the higher the risk, the greater the benefit from risk factor modification, including pharmacological interventions.Although some cardiovascular risk factors, such as age and genetic predisposition, are non-modifiable, modifying dyslipidaemia, hypertension, diabetes mellitus and smoking can drastically improve long-term prognosis.In the primary analysis of the prospective SPRINT trial91involving 9,361 patients with hypertension but no diabetes, intensive blood pressure lowering to <120 mmHg was associated with a reduced risk of MACEs (primary myocardial infarction, other acute coronary syndrome, stroke, heart failure or death from cardiovascular causes) compared with standard therapy (HR 0.73, 95% CI 0.60–0.90).Similarly, the primary analysis of the ADVANCE trial96showed that intensive glycaemic control reduced MACEs (cardiovascular causes, non-fatal myocardial infarction or non-fatal stroke) compared with standard control (HR 0.86, 95% CI 0.77–0.97) in 11,140 patients with type 2 diabetes.
However, some clinical risk factors are not well captured by conventional risk algorithms, including obesity, physical inactivity, metabolic syndrome, chronic kidney disease, immune-mediated inflammatory diseases, psychosocial stress, psychiatric disorders, social deprivation and frailty97,,,,98,,,,99。Moreover, a high proportion of asymptomatic individuals undergoing CCTA in population-based screening studies, such as the MIAMI Heart Study64and SCAPIS96cohorts, had subclinical atherosclerosis, despite seemingly low 10-year event risk calculations.In addition, the optimal treatment of patients with a borderline indication for statins is often unclear, and most individuals who present with acute myocardial infarction do not have a history of angina or other symptoms that could herald their underlying condition.Therefore, a need exists for more refined risk stratification than can be achieved through the assessment of clinical risk factors alone.In the SCOT-HEART trial100, the use of CCTA led to greater diagnostic certainty and risk stratification, with increased use of procedural and pharmacological interventions, compared with standard care despite similar 10-year cardiovascular risk scores between groups.Crucially, this finding was independent of the presentation of symptoms, with the greatest benefit seen in patients without angina owing to coronary heart disease100。These data suggest that CCTA could be a powerful clinical adjunct for assessing total cardiovascular risk in asymptomatic individuals with risk factors.This hypothesis is the subject of the ongoing, randomized SCOT-HEART 2 study101, in which the investigators will assess whether CCTA-guided care leads to improvements in management and outcomes in patients with stable angina and suspected CAD after a 10-year follow-up period.
Surrounding adipose tissue
CCTA-derived metrics of fat surrounding the coronary arteries and heart represent promising markers of inflammation, a key mechanism in atherosclerosis102。On non-contrast CT scans, standardized at 120 kVp for calcium scoring, increased volume of epicardial adipose tissue is linked to an increased risk of cardiovascular events, offering predictive value beyond the CAC score103。Although previously constrained by lengthy segmentation processes, advances in AI-supported software now enable automated evaluation of epicardial adipose tissue104。Moreover, on CCTA, pericoronary adipose tissue (PCAT) attenuation can be quantified105。PCAT is currently incorporated into proprietary measurements and risk scores, which may add prognostic value106。In the ORFAN study106cohort of 40,091 patients with a clinical indication for CCTA, the PCAT attenuation score was independently associated with cardiovascular mortality (HR 29.8, 95% CI 13.9–63.9) and MACEs (myocardial infarction, new heart failure and cardiac death; HR 12.6, 95% CI 8.5–18.6) irrespective of CAD severity, although this PCAT score contributed only marginally to the area under the curve.Moreover, the difference in PCAT attenuation values between healthy and stenosed arteries is subtle105, and PCAT attenuation measurements are affected by tube voltage, image reconstruction kernel and iterative reconstruction techniques, which can result in attenuation differences far greater than those between healthy and diseased vessels107,,,,108。Further validation of epicardial adipose tissue and PCAT for clinical decision-making in a prospective, randomized, controlled, cardiovascular outcomes trial is required to determine the clinical value for individualized management102。
AI in atherosclerosis imaging
Applications and limitations
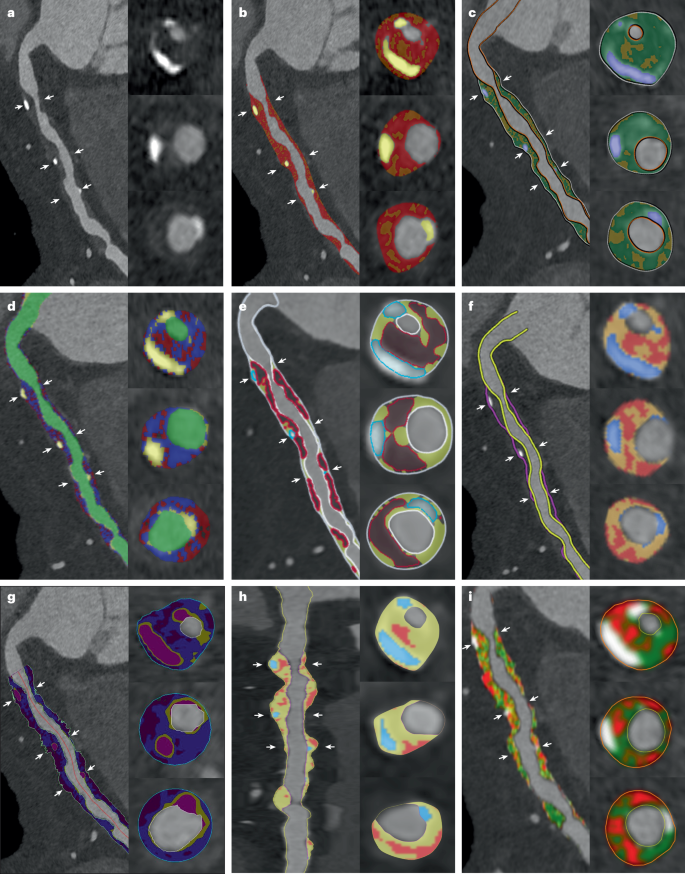
AI and ML are transforming the landscape of atherosclerotic cardiovascular risk assessment: first, through the direct application of deep learning algorithms to image data for automated quantification of imaging biomarkers, such as atherosclerotic plaque24, and second, by combining clinical and AI-supported imaging metrics for individualized outcome prediction31。Applications for deep learning models in cardiac CT are diverse and include CAC quantification on non-contrast CT109,,,,110,,,,111, quantification of CAD Reporting and Data System score, identification of atherosclerotic plaque type and atherosclerotic plaque quantification on CCTA (Fig. 5)。Fully automated, deep learning methods for atherosclerotic plaque and vessel lumen segmentation promise to provide accelerated quantification, saving the reader time19。
Each panel shows a multiplanar reformation of the right coronary artery along three axial cross-sections with overlayed segmentation of calcified plaque, non-calcified plaque and low-attenuation plaque.The positions of the cross-sections are denoted by white arrows.Quantification of atherosclerotic coronary plaque modestly improved event prediction compared with atherosclerotic cardiovascular disease risk score alone53。Analysis was performed using eight different commercially available systems approved by the FDA25。一个, 参考。b, AutoPlaque version 3.0 (Cedars–Sinai Medical Center, USA).c, syngo.via Frontier Coronary Analysis Prototype version 1.0.3 (Siemens Healthineers).d, Vitrea Sure Plaque Analysis version 7.16 (Canon Medical Systems).e, PlaqueIQ (Elucid Bioimaging).f, Artrya Salix Coronary Plaque (RUO) version 1.0 (Artrya).g, Aquarius iNtuition version 4.10 (TeraRecon).h, Cleerly LABS version 2.0 (Cleerly).我, QAngio CT Research Edition version 3.2.14.1 (Medis Medical Imaging).Heartflow was unable to provide the required analysis for inclusion in the publication.The orientation in part一个was supplied as a visual reference to all vendors.In a retrospective analysis of 1,611 patients from the SCOT-HEART trial, a deep learning-supported method for atherosclerotic plaque quantification on CCTA was shown to be concordant with IVUS and also predictive of myocardial infraction
19。The deep learning-based TPV threshold was associated with an increased risk of myocardial infarction (HR 5.36, 95% CI 1.70–16.86) after adjustment for the presence of deep learning-based obstructive stenosis (HR 2.49, 95% CI 1.07–5.50) and the ASSIGN clinical risk score (HR 1.01, 95% CI 0.99–1.04)15。In the ISCHEMIA trial72, CCTA data were available from 3,711 participants with myocardial ischaemia.AI-based TPV was associated with cardiovascular death or myocardial infarction (HR 1.56, 95% CI 1.25–1.97 per interquartile range increase (559 mm3)), with atherosclerotic plaque volume and composition metrics modestly improving event prediction compared with ASCVD risk score alone72。Owing to the inclusion of patients who had previously undergone percutaneous coronary intervention and the limited image quality in this study, further randomized controlled trials are needed to support these findings.
The main challenge associated with AI tools is the limited availability of the large, well-curated and diverse data sets required for training and generalizability112。A wide range of scanners and scan protocols should be included in training data to improve performance.As with other diagnostic approaches, deep learning-supported methods must be evaluated before integration with the corresponding invasive reference standards, such as IVUS for atherosclerotic plaque quantification, and also externally with fully independent data25。High image quality (and the absence of artefacts) is central to quantitative assessment of atherosclerotic plaque and, together with vessel size, determines whether quantitative analysis of atherosclerotic plaque should be performed for that vessel segment25。
可靠性
AI-supported CCTA quantification of atherosclerotic plaque has been compared with assessment by human readers and using IVUS.The reliability of AI tools between scans performed at short intervals was also evaluated.Agreement between AI tools and expert human readers is excellent (intraclass correlation coefficient (ICC) 0.96)19。However, wide limits of agreement between humans and AI (–114 mm3to 126 mm3) have been reported, although this range is narrower than between two human readers (–157 mm3to 203 mm3)19。Agreement with experts is best for TPV (ICC 0.96) and worst for low-density NCP (ICC 0.81).AI-supported quantification of atherosclerotic plaque also shows excellent agreement with IVUS for TPV (r = 0.91), NCPV (r = 0.87) and CPV (r = 0.91), but poor agreement for low-density NCP (r = 0.28)27。Interscan reliability is also good and, again, better for TPV, NCPV and CPV (r = 0.93–0.98) than for low-density NCP (r = 0.74)65,,,,113。The reliability of AI tools is not without limitations.Although population-level agreement is good, limits of agreement between scan and rescan are wide (±50% for TPV, NCPV and CPV and ±100% for low-density NCP
55,,,,96)。These findings mean that, for individual patient follow-up, it is not possible to determine whether shifts in atherosclerotic plaque volume of up to 50% represent response to therapy, disease progression or simply interscan variability.This effect is further compounded by intersoftware variability.An evaluation of various software packages on a single vessel demonstrated that the TPV (normalized to vessel volume) ranged from 58% to 88% across software vendors, NCPV ranged from 75% to 99% and the proportion of low-density NCP varied from 0.3% to 35% of the TPV25。This variability has important clinical implications for patients whose scores fall near the thresholds of risk categories and who could be reclassified solely on the basis of the software used for their scans on different days.
Individualized recommendations for medical treatment
指标
Population-based CCTA studies, such as the Multi-Ethnic Study of Atherosclerosis66and the subsequent Miami Heart Study68,,,,114, have greatly advanced our knowledge of atherosclerotic plaque prevalence and its association with cardiovascular events.The 2018 multisociety clinical guideline on the management of blood cholesterol recommends using CAC scores to guide decisions on statin therapy for adults aged 40–75 years without diabetes, LDL-C concentration of 70–189 mg/dl (1.81–4.89 mmol/l) and a 10-year ASCVD risk of 7.5–20% when the need for statins is unclear36。If the CAC score is 0, statin therapy can generally be delayed, except for patients who smoke or those with diabetes or a strong family history of premature heart disease36。
CCTA is a first-line test in patients with chest pain and can visualize both the coronary artery lumen and atherosclerotic plaque (calcified and non-calcified), including the high-risk, low-attenuation component of NCP.In the SCOT-HEART trial7, women presenting with stable chest pain had lower atherosclerotic plaque volumes of all subtypes than men, although quantitative low-attenuation plaque burden was as strong a predictor of subsequent myocardial infarction in both women and men115。As a consequence, fixed cut-off values for atherosclerotic plaque volumes have been proposed for risk stratification73,,,,116,,,,117,,,,118。However, atherosclerotic plaque distribution is known to vary according to age and gender and, therefore, requires a wide range of cut-off values.Age-specific and gender-specific percentile thresholds have been proposed in two separate studies with different AI software applications for atherosclerotic plaque analysis29,,,,119。In a 2024 study29, per-patient age-specific and gender-specific atherosclerotic plaque distributions were shown to be strongly predictive of myocardial infarction, with the highest risk seen in patients with coronary plaque volumes above the 75th percentile (HR 2.65, 95% CI 1.47–4.78).Therefore, percentiles adjusted for age and gender could provide context to better interpret risk assessment from atherosclerotic plaque imaging and allow practical, individualized clinical treatment recommendations.In contrast to large deviations in proposed cut-off values73,,,,116,,,,117, two multicentre studies on different patient cohorts showed similarities between the age-adjusted and gender-adjusted percentile curves29,,,,119(Fig. 6)。
A treatment paradigm based on population distribution percentiles was deemed by the QCI Study Group to be the most suitable approach for medical treatment recommendations, with the 70th percentile being the threshold for recommending high-intensity treatment and the presence of any atherosclerotic plaque for standard-dose medical treatment (Fig. 4)。Although the percentile distributions from both studies follow similar trajectories, very divergent patient groups (in terms of ethnicities or risk profiles) could have greater differences in atherosclerotic plaque distributions.Further research is needed on whether treatment recommendations derived from average atherosclerotic plaque distribution can be effectively translated from one end of the spectrum of risk to the other.
Medical therapies and dose intensity
The aim of pharmacological management of chronic coronary syndrome is to prevent MACEs and to alleviate ischaemic symptoms.Central to this management strategy is the optimization of cardiovascular risk factors.Lifestyle interventions, such as diet modification and exercise, serve as basic measures, but are often insufficient to achieve the stringent LDL-C targets recommended for high-risk patients with chronic coronary syndrome.Effective blood pressure control in the general population and precise glucose level management in patients with diabetes are essential to reduce vascular complications and associated risk.The antihypertensive agents olmesartan and amlodipine have been shown to have beneficial effects on atherosclerotic plaque progression120,,,,121。Medications indicated for diabetes, such as sodium–glucose cotransporter 2 inhibitors and glucagon-like peptide 1 receptor agonists, are also thought to have beneficial effects on CAD progression and could have a role in future treatment strategies122。
Statins are the cornerstone of pharmacological lipid-lowering strategies, with a central role in reducing atherogenic burden and the occurrence of MACEs through LDL-C reduction, and secondary benefits such as atherosclerotic plaque stabilization and modulation of inflammation.The 2023 American123and 2024 European124guidelines emphasize the importance of LDL-C lowering and advocate for precise targets based on individual risk profiles.Both guidelines reinforce the treat-to-target paradigm, specifying both percentage-based LDL-C reductions and absolute thresholds for patients with chronic coronary syndrome.Meta-analyses of data from patients with stable CAD or acute coronary syndrome, in trials comparing statins versus no statin or low-dose versus high-dose statin theapy125,,,,126, have revealed that standard-intensity statin therapy effectively reduces MACEs (coronary death, myocardial infarction, coronary revascularization and ischaemic stroke), but is inferior to high-intensity statin therapy125。The recommendations from the QCI Study Group for standard-intensity and high-intensity statin regimens are summarized in Table 1。These recommendations on statin doses should be supplemented with adequate guideline-adherent lifestyle changes, antihypertensive therapy and antiplatelet therapy, if indicated.
Although statins are the first-line lipid-lowering therapy, other medications, such as cholesterol-absorption inhibitors (ezetimibe) and proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, are potential adjunctive treatments for patients who are at very high risk or unable to achieve the required LDL-C goals, despite the maximum-tolerated statin dose.PCSK9 inhibitors, such as alirocumab and evolocumab, markedly lower LDL-C levels by up to 60% when used in combination with statins127,,,,128,,,,129,,,,130。Other lipid-lowering agents available or currently under investigation, such as bempedoic acid, monoclonal antibodies (canakinumab)124and small interfering RNA-based agents (inclisiran), hold promise for the future individualization of CAD management, although data are not yet available from CCTA-based clinical studies evaluating their effects on atherosclerotic plaque.
Percentile-based treatment recommendations
The presence of atherosclerotic plaque, even if non-obstructive, detected by CCTA is associated with increased cardiovascular risk.The majority of the QCI Study Group members voted for a ‘treat any plaque’ strategy (Fig. 4), involving standard-intensity medical treatment after the detection of any atherosclerotic plaque, irrespective of size or composition.This strategy was found to be beneficial for patients in the prospective, randomized, controlled SCOT-HEART3and DISCHARGE7,,,,8trials.As recommended in international guidelines, dose escalation might be warranted for stronger lipid-lowering and anti-atherosclerotic effects.However, many individuals with elevated LDL-C levels, but no signs of atherosclerosis, will not have a cardiovascular event43,,,,131, suggesting that a treatment paradigm based on atherosclerotic plaque quantification rather than surrogate markers could improve patient outcome122。The QCI Study Group defined the TPV threshold for treatment escalation to high-intensity treatment as the age-adjusted and gender-adjusted 70th percentile (Fig. 4)。
Clinical risk factors and other atherosclerotic plaque features also have a pivotal role in risk modulation.Smoking, a positive family history of CVD, the presence of low-attenuation plaque and positive remodelling were deemed to be the most important factors in the decision to escalate towards high-intensity treatment (Fig. 4)。By contrast, very small fibrotic and calcified plaques almost never cause cardiovascular events and, consequently, allow for the de-escalation of medical treatment recommendations.
Limitations and future directions
Although consensus was reached on treatment percentiles, the Delphi process did not produce a unanimous position on the treatment of any atherosclerotic plaque.Standard-intensity medical treatment addresses the underlying pathophysiology of atherosclerosis, reduces the risk of cardiovascular events and stabilizes existing atherosclerotic plaques.However, with advances in scanner technology and increased scan availability, detecting small atherosclerotic plaques in patients with stable chest pain, or even healthy individuals, with low cardiovascular risk will become more common.Therefore, defining an optimal treatment threshold might be warranted in the future.The integration of NCP also proved to be a divisive topic, and no consensus could be reached.Although agreement was reached that NCP should not be disregarded, its role in individualized treatment recommendations and monitoring of treatment response is yet to be determined on the basis of data from future randomized trials.
AI in plaque assessment
Research shows that fully automated AI methods for the analysis of atherosclerotic plaque in conventional, single-energy CT perform at the level of inter-observer agreement with fast inferences19,,,,26,,,,132。Further advances in the robustness and resilience of these methods have the potential to bring the analysis to clinical use.Crucially, AI-supported analysis of CT imaging depends on high image quality, and a novel treatment paradigm based on AI-supported quantification of TPV requires accurate detection of atherosclerotic plaque.Owing to limited spatial resolution of CCTA, atherosclerotic plaque quantification is recommended only in vessels with a diameter >2 mm (refs.25,,,,93)。In addition, the presence of artefacts and noise can impede detailed delineation of plaque contours.For example, blooming of calcified components can affect the accurate characterization of adjacent low-attenuation plaque16。Variations in scanner systems and acquisition protocols affect atherosclerotic plaque characterization, presenting challenges for the accurate quantification of atherosclerotic plaques near to intensity-based cut-off points.Efforts to standardize CT acquisition and analysis are crucial to mitigate such differences25,,,,132。
Advances in CT image reconstruction133and photon-counting CT technology are expected to substantially advance the imaging of atherosclerotic plaque in the near future, owing to increased spatial resolution134and spectral capabilities135。Nevertheless, the application of AI-supported analysis of these novel CT images will be associated with new challenges, mainly concerning optimal image reconstruction and the exploitation of multienergy level imaging136。Further development of existing AI methods for use with (spectral) photon-counting CT could involve the handling of large and high-dimensional data.In the next few years, advances in AI technologies could unlock the potential for the improved analysis of atherosclerotic plaque anatomy and easier identification of vulnerable plaque, facilitating individualized treatment recommendations.
Clinical implications
The increased use of AI-supported coronary atherosclerosis imaging will generate unprecedented volumes of data.The challenge will be to integrate these data into meaningful information for effective guidance of patient management.We should resist the temptation to generate hypotheses based on the data but instead focus on testing hypotheses that are firmly grounded in our understanding of CAD pathophysiology.By integrating quantitative assessments of coronary plaque burden, composition and progression, advanced algorithms for patient management have the potential to deliver truly individualized treatment, considering crucial factors such as ethnic variability, comorbidities and concurrent therapies.
Given the expanding options for medical therapy, with the growing armamentarium of lipid-lowering and anti-inflammatory therapies, a need clearly exists to individualize treatment intensity.The relationship among disease burden, inflammatory activity and atherosclerotic plaque progression must guide these advances, because they are the key determinants of cardiovascular risk.AI-supported imaging, incorporating age-adjusted and gender-adjusted TPV percentiles, could provide a foundation to refine treatment thresholds.Inflammatory markers and coronary imaging risk modifiers could inform the treatment intensity required to halt disease progression.Finally, atherosclerotic plaque characteristics will add nuanced adjustments to optimize treatment.The effectiveness of these innovative approaches must be rigorously validated through well-designed, prospective, randomized, controlled clinical trials.This requirement presents a major challenge, given the many options for tailored management and the need for individual effectiveness research.The recommendations contained in this Consensus Statement could provide a foundation for these trials.
结论
AI-supported tools to evaluate atherosclerotic plaque offer the potential to refine the precision of risk stratification and improve clinical decision-making by providing reliable and accurate assessments of atherosclerotic plaque burden and morphology.The QCI Study Group deemed the age-adjusted and gender-adjusted percentiles of TPV to be the most meaningful parameter for the individualized initiation and escalation of medical treatment.TPV is a major risk predictor for MACEs and outperforms other atherosclerotic plaque subtype metrics, such as CPV or NCPV, as well as providing modest independent discrimination in addition to cardiovascular risk factors72。Treatment escalation to high-intensity regimens is recommended for patients with TPV above the 70th percentile.Clinical risk factors and high-risk plaque features can also inform decisions on treatment escalation.
The implementation of individualized treatment recommendations, guided by AI-supported assessment of coronary atherosclerotic plaque, represents a substantial paradigm shift in cardiovascular risk management.Although these consensus recommendations provide a practical framework for integrating AI-supported evaluation of atherosclerotic plaque into routine clinical practice, further large-scale, randomized, controlled cardiovascular outcome trials integrating novel anti-atherosclerotic agents are necessary to validate these recommendations.This evolving approach highlights the growing importance of advanced imaging of coronary atherosclerosis biomarkers and AI-driven analysis as companion diagnostics in transforming cardiovascular care, moving from generalized risk scoring to individualized treatment pathways based on coronary atherosclerotic plaque morphology and should be tested in trials of CT versus CT with AI.
参考
Weir-McCall, J. R. et al.National trends in coronary artery disease imaging: associations with health care outcomes and costs.JACC Cardiovasc.成像 16, 659–671 (2023).
Schmidt, M. et al.The Western Denmark Heart Registry: its influence on cardiovascular patient care.J. Am.科尔。Cardiol. 71, 1259–1272 (2018).
Langenbach, M. C. et al.German Radiological Society and the Professional Association of German Radiologists Position Paper on coronary computed tomography: clinical evidence and quality of patient care in chronic coronary syndrome.Rofo 195, 115–134 (2023).
van den Boogert, T. P. W. et al.The impact and challenges of implementing CTCA according to the 2019 ESC guidelines on chronic coronary syndromes: a survey and projection of CTCA services in the Netherlands.Insights Imaging 12, 186 (2021).
Dewey, M. et al.Evaluation of computed tomography in patients with atypical angina or chest pain clinically referred for invasive coronary angiography: randomised controlled trial.BMJ 355, i5441 (2016).
Mézquita, A. J. V. et al.Clinical quantitative coronary artery stenosis and coronary atherosclerosis imaging: a Consensus Statement from the Quantitative Cardiovascular Imaging Study Group.纳特。Rev. Cardiol. 20, 696–714 (2023).
The SCOT-HEART Investigators.Coronary CT angiography and 5-year risk of myocardial infarction.N. Engl.J. Med. 379, 924–933 (2018).The SCOT-HEART and DISCHARGE trials were key studies that changed reimbursement paradigms in Europe and beyond.Analysis of data from both trials was used to inform the selection of participants to choose optimal treatment thresholds.
The DISCHARGE Trial Group.CT or invasive coronary angiography in stable chest pain.N. Engl.J. Med. 386, 1591–1602 (2022).
Williams, M. C. et al.Coronary CT angiography-guided management of patients with stable chest pain: 10-year outcomes from the SCOT-HEART randomised controlled trial in Scotland.Lancet 405, 329–337 (2025).
Adamson, P. D. & Newby, D. E. The SCOT-HEART trial.What we observed and what we learned.J. Cardiovasc。Comput.Tomogr. 13, 54–58 (2019).
Doenst, T. et al.PCI and CABG for treating stable coronary artery disease: JACC review topic of the week.J. Am.科尔。Cardiol. 73, 964–976 (2019).
Doenst, T., Bonow, R. O., Bhatt, D. L., Falk, V. & Gaudino, M. Improving terminology to describe coronary artery procedures: JACC review topic of the week.J. Am.科尔。Cardiol. 78, 180–188 (2021).
Napp, A. E. et al.Computed tomography versus invasive coronary angiography: design and methods of the pragmatic randomised multicentre DISCHARGE trial.Eur.Radiol. 27, 2957–2968 (2017).
The DISCHARGE Trial Group.Comparative effectiveness of initial computed tomography and invasive coronary angiography in women and men with stable chest pain and suspected coronary artery disease: multicentre randomised trial.BMJ 379, e071133 (2022).
The DISCHARGE Trial Group.Age and computed tomography and invasive coronary angiography in stable chest pain: a prespecified secondary analysis of the DISCHARGE randomized clinical trial.贾马心脏。 9, 346–356 (2024).
Williams, M. C., Earls, J. P. & Hecht, H. Quantitative assessment of atherosclerotic plaque, recent progress and current limitations.J. Cardiovasc。Comput.Tomogr. 16, 124–137 (2022).
Trost, J. et al.CCTA should be the new diagnostic gateway for evaluating intermediate-risk stable angina patients.JACC Adv. 1, 100116 (2022).
Maurovich-Horvat, P., Ferencik, M., Voros, S., Merkely, B. & Hoffmann, U. Comprehensive plaque assessment by coronary CT angiography.纳特。Rev. Cardiol. 11, 390–402 (2014).
Lin, A. et al.Deep learning-enabled coronary CT angiography for plaque and stenosis quantification and cardiac risk prediction: an international multicentre study.Lancet Digit.健康 4, e256–e265 (2022).This externally validated, deep learning system demonstrated that AI-supported analysis of atherosclerotic plaque on coronary CT angiography agrees closely with expert readers and intravascular ultrasonography and could have prognostic value for predicting future myocardial infarction.
CAS一个 Google Scholar一个
Föllmer, B. et al.Roadmap on the use of artificial intelligence for imaging of vulnerable atherosclerotic plaque in coronary arteries.纳特。Rev. Cardiol. 21, 51–64 (2024).
Varoquaux, G. & Cheplygina, V. Machine learning for medical imaging: methodological failures and recommendations for the future.npj Digit.医学 5, 48 (2022).
Lin, A. et al.Artificial intelligence in cardiovascular imaging for risk stratification in coronary artery disease.Radiol.Cardiothorac.成像 3, e200512 (2021).
van Herten, R. L. M., Lagogiannis, I., Leiner, T. & Išgum, I. The role of artificial intelligence in coronary CT angiography.Neth.Heart J. 32, 417–425 (2024).
Nannini, G. et al.A fully automated deep learning approach for coronary artery segmentation and comprehensive characterization.APL Bioeng. 8, 016103 (2024).
Nieman, K. et al.Standards for quantitative assessments by coronary computed tomography angiography (CCTA): an expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT).J. Cardiovasc。Comput.Tomogr. 18, 429–443 (2024).This SCCT consensus document emphasizes the standardization of AI-supported analysis of atherosclerotic plaque in coronary artery disease, thereby serving as the counterpart to the proposed individualization.
Herten, V. et al.Automatic coronary artery plaque quantification and CAD-RADS prediction using mesh priors.IEEE Trans.医学成像 43, 1272–1283 (2024).
Narula, J. et al.Prospective deep learning-based quantitative assessment of coronary plaque by computed tomography angiography compared with intravascular ultrasound: the REVEALPLAQUE study.Eur.Heart J. Cardiovasc.成像 25, 1287–1295 (2024).
Jie, P. et al.Diagnostic value of artificial intelligence-assisted CTA for the assessment of atherosclerosis plaque: a systematic review and meta-analysis.正面。Cardiovasc.医学 11, 1398963 (2024).
Miller, R. J. H. et al.Patient-specific myocardial infarction risk thresholds from AI-enabled coronary plaque analysis.Circ.Cardiovasc.成像 17, e016958 (2024).This article demonstrated that age-adjusted and gender-adjusted percentile curves of atherosclerotic plaque volumes are predictive of cardiovascular events.
Dewey, M. The future of radiology: adding value to clinical care.Lancet 392, 472–473 (2018).
Nurmohamed, N. S. et al.AI-guided quantitative plaque staging predicts long-term cardiovascular outcomes in patients at risk for atherosclerotic CVD.JACC Cardiovasc.成像 17, 269–280 (2024).
Williams, M. C. et al.Low-attenuation noncalcified plaque on coronary computed tomography angiography predicts myocardial infarction: results from the multicenter SCOT-HEART trial (Scottish Computed Tomography of the HEART).循环 141, 1452–1462 (2020).
CAS一个 Google Scholar一个
Budoff, M. J. et al.Effect of icosapent ethyl on progression of coronary atherosclerosis in patients with elevated triglycerides on statin therapy: final results of the EVAPORATE trial.Eur.Heart J. 41, 3925–3932 (2020).
CAS一个 Google Scholar一个
Nieman, K. et al.Multislice computed tomography angiography for noninvasive assessment of the 18-month performance of a novel radiolucent bioresorbable vascular scaffolding device: the ABSORB trial (a clinical evaluation of the bioabsorbable everolimus eluting coronary stent system in the treatment of patients with de novo native coronary artery lesions).J. Am.科尔。Cardiol. 62, 1813–1814 (2013).
Corrigendum to: 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk.Eur.Heart J。41, 4255 (2020).Grundy, S. M. et al.
2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines.J. Am.科尔。Cardiol. 73, e285–e350 (2019).
Martin, S. S. et al.2024 heart disease and stroke statistics: a report of US and global data from the American Heart Association.循环 149, e347–e913 (2024).
Di Cesare, M. et al.World Heart Report 2023: confronting the world’s number one killer.World Heart Federation https://world-heart-federation.org/wp-content/uploads/World-Heart-Report-2023.pdf(2023)。
Akosah, K. O., Schaper, A., Cogbill, C. & Schoenfeld, P. Preventing myocardial infarction in the young adult in the first place: how do the National Cholesterol Education Panel III guidelines perform?J. Am.科尔。Cardiol. 41, 1475–1479 (2003).
Bautista, L. E. & Rueda-Ochoa, O. L. Methodological challenges in studies of the role of blood lipids variability in the incidence of cardiovascular disease.Lipids Health Dis. 20, 51 (2021).
Zaman, S. et al.The Lancet Commission on rethinking coronary artery disease: moving from ischaemia to atheroma.Lancet405 , 1264–1312 (2025).Google Scholar
一个 Bittner, D. O. et al.
Influence of cardiovascular risk factors on the prevalence of coronary atherosclerosis in patients with angiographically normal coronary arteries.Acad.Radiol. 24, 580–586 (2017).
Mortensen, M. B. et al.Low-density lipoprotein cholesterol is predominantly associated with atherosclerotic cardiovascular disease events in patients with evidence of coronary atherosclerosis: the Western Denmark Heart Registry.循环 147, 1053–1063 (2023).
CAS一个 Google Scholar一个
Reynolds, H. R. et al.Outcomes in the ISCHEMIA trial based on coronary artery disease and ischemia severity.循环 144, 1024–1038 (2021).
CAS一个 Google Scholar一个
Karpe, F. & Holman, R. Fire-and-forget in prevention of coronary heart disease.Lancet 360, 1984 (2002).
Dewey, M. et al.Clinical quantitative cardiac imaging for the assessment of myocardial ischaemia.纳特。Rev. Cardiol. 17, 427–450 (2020).
Stary, H. C. et al.A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis.A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association.循环 92, 1355–1374 (1995).
CAS一个 Google Scholar一个
Jebari-Benslaiman, S. et al.Pathophysiology of atherosclerosis.int。J. Mol。科学。 23, 47 (2022).
Biavati, F. et al.Coronary artery calcium score predicts major adverse cardiovascular events in stable chest pain.Radiology 310, e231557 (2024).
Pinto-Sietsma, S. J., Velthuis, B. K., Nurmohamed, N. S., Vliegenthart, R. & Martens, F. Computed tomography and coronary artery calcium score for screening of coronary artery disease and cardiovascular risk management in asymptomatic individuals.Neth.Heart J. 32, 371–377 (2024).
Valenti, V. et al.A 15-year warranty period for asymptomatic individuals without coronary artery calcium: a prospective follow-up of 9,715 individuals.JACC Cardiovasc.成像 8, 900–909 (2015).
Blaha, M. J. et al.Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis (MESA).循环 133, 849–858 (2016).
CAS一个 Google Scholar一个
Sandesara, P. B. et al.Clinical significance of zero coronary artery calcium in individuals with LDL cholesterol ≥190 mg/dl: the multi-ethnic study of atherosclerosis.Atherosclerosis 292, 224–229 (2020).
CAS一个 Google Scholar一个
van der Aalst, C. M. et al.Screening for cardiovascular disease risk using traditional risk factor assessment or coronary artery calcium scoring: the ROBINSCA trial.Eur.Heart J. Cardiovasc.成像 21, 1216–1224 (2020).
Mitchell, J. D. et al.Impact of statins on cardiovascular outcomes following coronary artery calcium scoring.J. Am.科尔。Cardiol. 72, 3233–3242 (2018).
CAS一个 Google Scholar一个
Miedema, M. D. et al.Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis.Circ.Cardiovasc.素质。结果 7, 453–460 (2014).
Indraratna, P. et al.Aspirin and statin therapy for nonobstructive coronary artery disease: five-year outcomes from the CONFIRM registry.Radiol.Cardiothorac.成像 4, e210225 (2022).
Rozanski, A. et al.Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) prospective randomized trial.J. Am.科尔。Cardiol. 57, 1622–1632 (2011).
CAS一个 Google Scholar一个
van Rosendael, A. R. et al.Association of high-density calcified 1 K plaque with risk of acute coronary syndrome.贾马心脏。 5, 282–290 (2020).
Hussain, A., Ballantyne, C. M. & Nambi, V. Zero coronary artery calcium score: desirable, but enough?循环 142, 917–919 (2020).
Budoff, M. J. et al.Prognostic value of coronary artery calcium in the PROMISE study (Prospective Multicenter Imaging Study for Evaluation of Chest Pain).循环 136, 1993–2005 (2017).
CAS一个 Google Scholar一个
Di Giovanni, G., Kataoka, Y., Bubb, K., Nelson, A. J. & Nicholls, S. J. Impact of lipid lowering on coronary atherosclerosis moving from the lumen to the artery wall.Atherosclerosis 367, 8–14 (2023).
Houslay, E. S. et al.Progressive coronary calcification despite intensive lipid-lowering treatment: a randomised controlled trial.心 92, 1207–1212 (2006).
CAS一个 Google Scholar一个
Nadjiri, J. et al.Incremental prognostic value of quantitative plaque assessment in coronary CT angiography during 5 years of follow up.J. Cardiovasc。Comput.Tomogr. 10, 97–104 (2016).
Meah, M. N. et al.Plaque burden and 1-year outcomes in acute chest pain: results from the multicenter RAPID-CTCA trial.JACC Cardiovasc.成像 15, 1916–1925 (2022).
van Rosendael, A. R. et al.Association of statin treatment with progression of coronary atherosclerotic plaque composition.贾马心脏。 6, 1257–1266 (2021).
Lu, M. T. et al.Effects of pitavastatin on coronary artery disease and inflammatory biomarkers in HIV: mechanistic substudy of the REPRIEVE randomized clinical trial.贾马心脏。 9, 323–334 (2024).
Nasir, K. et al.Coronary atherosclerosis in an asymptomatic U.S. population: Miami Heart Study at Baptist Health South Florida.JACC Cardiovasc.成像 15, 1604–1618 (2022).
Fuchs, A. et al.Subclinical coronary atherosclerosis and risk for myocardial infarction in a Danish cohort: a prospective observational cohort study.安。实习生。医学 176, 433–442 (2023).
Hoffmann, U. et al.Prognostic value of noninvasive cardiovascular testing in patients with stable chest pain: insights from the PROMISE trial (Prospective Multicenter Imaging Study for Evaluation of Chest Pain).循环 135, 2320–2332 (2017).
Singh, T. et al.Exercise electrocardiography and computed tomography coronary angiography for patients with suspected stable angina pectoris: a post hoc analysis of the randomized SCOT-HEART trial.贾马心脏。 5, 920–928 (2020).
Nurmohamed, N. S. et al.Atherosclerosis quantification and cardiovascular risk: the ISCHEMIA trial.Eur.Heart J. 45, 3735–3747 (2024).Results from the ISCHEMIA trial demonstrated that total plaque volume has incremental value for patient management compared with conventional visual coronary CT angiography.
Deseive, S. et al.Quantified coronary total plaque volume from computed tomography angiography provides superior 10-year risk stratification.Eur.Heart J. Cardiovasc.成像 22, 314–321 (2021).
Bell, J. S. et al.Plaque quantification from coronary computed tomography angiography in predicting cardiovascular events: a systematic review and meta-analysis.J. Cardiovasc。Comput.Tomogr. https://doi.org/10.1016/j.jcct.2025.05.003(2025).
Vergallo, R. et al.Vulnerable or high-risk plaque: a JACC: Cardiovascular Imaging Position Statement.JACC Cardiovasc.成像 18, 709–740 (2025).
Nerlekar, N. et al.Computed tomographic coronary angiography-derived plaque characteristics predict major adverse cardiovascular events: a systematic review and meta-analysis.Circ.Cardiovasc.成像 11, e006973 (2018).
Pflederer, T. et al.Characterization of culprit lesions in acute coronary syndromes using coronary dual-source CT angiography.Atherosclerosis 211, 437–444 (2010).
CAS一个 Google Scholar一个
Hoffmann, U. et al.Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable lesions in stable angina by multidetector computed tomography.J. Am.科尔。Cardiol. 47, 1655–1662 (2006).
Kitagawa, T. et al.Characterization of noncalcified coronary plaques and identification of culprit lesions in patients with acute coronary syndrome by 64-slice computed tomography.JACC Cardiovasc.成像 2, 153–160 (2009).
Kataoka, Y. et al.Spotty calcification as a marker of accelerated progression of coronary atherosclerosis: insights from serial intravascular ultrasound.J. Am.科尔。Cardiol. 59, 1592–1597 (2012).
Ehara, S. et al.Spotty calcification typifies the culprit plaque in patients with acute myocardial infarction: an intravascular ultrasound study.循环 110, 3424–3429 (2004).
Motoyama, S. et al.Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome.J. Am.科尔。Cardiol. 54, 49–57 (2009).
Cademartiri, F. et al.Influence of intracoronary attenuation on coronary plaque measurements using multislice computed tomography: observations in an ex vivo model of coronary computed tomography angiography.Eur.Radiol. 15, 1426–1431 (2005).
Achenbach, S. et al.Influence of slice thickness and reconstruction kernel on the computed tomographic attenuation of coronary atherosclerotic plaque.J. Cardiovasc。Comput.Tomogr. 4, 110–115 (2010).
Ferencik, M. et al.Arterial wall imaging: evaluation with 16-section multidetector CT in blood vessel phantoms and ex vivo coronary arteries.Radiology 240, 708–716 (2006).
Suzuki, S. et al.Accuracy of attenuation measurement of vascular wall in vitro on computed tomography angiography: effect of wall thickness, density of contrast medium, and measurement point.投资。Radiol. 41, 510–515 (2006).
Otsuka, K. et al.Napkin-ring sign on coronary CT angiography for the prediction of acute coronary syndrome.JACC Cardiovasc.成像 6, 448–457 (2013).
Ferencik, M. et al.Use of high-risk coronary atherosclerotic plaque detection for risk stratification of patients with stable chest pain: a secondary analysis of the PROMISE randomized clinical trial.贾马心脏。 3, 144–152 (2018).
Maroules, C. D. et al.Coronary Artery Disease Reporting and Data System (CAD-RADS(TM)): inter-observer agreement for assessment categories and modifiers.J. Cardiovasc。Comput.Tomogr. 12, 125–130 (2018).
Ferencik, M. et al.A computed tomography-based coronary lesion score to predict acute coronary syndrome among patients with acute chest pain and significant coronary stenosis on coronary computed tomographic angiogram.是。J. Cardiol. 110, 183–189 (2012).
Puchner, S. B. et al.High-risk plaque detected on coronary CT angiography predicts acute coronary syndromes independent of significant stenosis in acute chest pain: results from the ROMICAT-II trial.J. Am.科尔。Cardiol. 64, 684–692 (2014).
Vattay, B. et al.Impact of virtual monoenergetic levels on coronary plaque volume components using photon-counting computed tomography.Eur.Radiol. 33, 8528–8539 (2023).
CAS一个 Google Scholar一个
Shaw, L. J. et al.Society of Cardiovascular Computed Tomography/North American Society of Cardiovascular Imaging — Expert Consensus Document on Coronary CT Imaging of Atherosclerotic Plaque.J. Cardiovasc。Comput.Tomogr. 15, 93–109 (2021).
Visseren, F. L. J. et al.2021 ESC Guidelines on cardiovascular disease prevention in clinical practice.Eur.Heart J. 42, 3227–3337 (2021).
Arnett, D. K. et al.2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: a report of the American College of Cardiology/American Heart Association Task force on Clinical Practice Guidelines.循环 140, e596–e646 (2019).
ADVANCE Collaborative Group.Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes.N. Engl.J. Med. 358, 2560–2572 (2008).
Talha, I., Elkhoudri, N. & Hilali, A. Major limitations of cardiovascular risk scores.Cardiovasc.ther。 2024, 4133365 (2024).
Wormser, D. et al.Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies.Lancet 377, 1085–1095 (2011).
Damen, J. A. et al.Prediction models for cardiovascular disease risk in the general population: systematic review.BMJ 353, i2416 (2016).
Adamson, P. D. et al.Guiding therapy by coronary CT angiography improves outcomes in patients with stable chest pain.J. Am.科尔。Cardiol. 74, 2058–2070 (2019).
McDermott, M. et al.Rationale and design of SCOT-HEART 2 trial.JACC Cardiovasc.成像 17, 1101–1112 (2024).
Grodecki, K. et al.Phenotyping atherosclerotic plaque and perivascular adipose tissue: signalling pathways and clinical biomarkers in atherosclerosis.纳特。Rev. Cardiol. 22, 443–455 (2025).
Spearman, J. V. et al.Prognostic value of epicardial fat volume measurements by computed tomography: a systematic review of the literature.Eur.Radiol. 25, 3372–3381 (2015).
Miller, R. J. H. et al.AI-derived epicardial fat measurements improve cardiovascular risk prediction from myocardial perfusion imaging.npj Digit.医学 7, 24 (2024).
Ma, R. et al.Evaluation of pericoronary adipose tissue attenuation on CT.br。J. Radiol. 96, 20220885 (2023).
Chan, K. et al.Inflammatory risk and cardiovascular events in patients without obstructive coronary artery disease: the ORFAN multicentre, longitudinal cohort study.Lancet 403, 2606–2618 (2024).
CAS一个 Google Scholar一个
Ma, R. et al.Towards reference values of pericoronary adipose tissue attenuation: impact of coronary artery and tube voltage in coronary computed tomography angiography.Eur.Radiol. 30, 6838–6846 (2020).
Lisi, C. et al.The pericoronary adipose tissue attenuation in CT strongly depends on kernels and iterative reconstructions.Eur.Radiol. 35, 2866–2876 (2025).
Pieszko, K. et al.Deep learning of coronary calcium scores from PET/CT attenuation maps accurately predicts adverse cardiovascular events.JACC Cardiovasc.成像 16, 675–687 (2023).
van Velzen, S. G. M. et al.Deep learning for automatic calcium scoring in CT: validation using multiple cardiac CT and chest CT protocols.Radiology 295, 66–79 (2020).
Föllmer, B. et al.Automated segment-level coronary artery calcium scoring on non-contrast CT: a multi-task deep-learning approach.Insights Imaging 15, 250 (2024).
Lekadir, K. et al.FUTURE-AI: international consensus guideline for trustworthy and deployable artificial intelligence in healthcare.BMJ 388, e081554 (2025).
Iraqi, N. et al.Interscan reproducibility of computed tomography derived coronary plaque volume measurements.J. Cardiovasc。Comput.Tomogr. 18, 583–592 (2024).
Blaha Michael, J. & DeFilippis Andrew, P. Multi-Ethnic Study of Atherosclerosis (MESA).J. Am.科尔。Cardiol. 77, 3195–3216 (2021).
CAS一个 Google Scholar一个
Williams, M. C. et al.Sex-specific computed tomography coronary plaque characterization and risk of myocardial infarction.JACC Cardiovasc.成像 14, 1804–1814 (2021).
van Diemen, P. A. et al.Prognostic value of RCA pericoronary adipose tissue CT-attenuation beyond high-risk plaques, plaque volume, and ischemia.JACC Cardiovasc.成像 14, 1598–1610 (2021).
Dundas, J. et al.Interaction of AI-enabled quantitative coronary plaque volumes on coronary CT angiography, FFRCT, and clinical outcomes: a retrospective analysis of the ADVANCE registry.Circ.Cardiovasc.成像 17, e016143 (2024).
Freeman, A. M. et al.Integrating coronary atherosclerosis burden and progression with coronary artery disease risk factors to guide therapeutic decision making.是。J. Med. 136, 260–269.e7 (2023).
CAS一个 Google Scholar一个
Tzimas, G. et al.Age- and sex-specific nomographic CT quantitative plaque data from a large international cohort.JACC Cardiovasc.成像 17, 165–175 (2024).
Hirohata, A. et al.Four-year clinical outcomes of the OLIVUS-Ex (impact of olmesartan on progression of coronary atherosclerosis: evaluation by intravascular ultrasound) extension trial.Atherosclerosis 220, 134–138 (2012).
CAS一个 Google Scholar一个
Nissen, S. E. et al.Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial.JAMA 291, 1071–1080 (2004).
CAS一个 Google Scholar一个
Dawson, L. P., Lum, M., Nerleker, N., Nicholls, S. J. & Layland, J. Coronary atherosclerotic plaque regression: JACC state-of-the-art review.J. Am.科尔。Cardiol. 79, 66–82 (2022).
Virani, S. S. et al.2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines.循环 148, e9–e119 (2023).
Vrints, C. et al.2024 ESC guidelines for the management of chronic coronary syndromes: developed by the task force for the management of chronic coronary syndromes of the European Society of Cardiology (ESC) endorsed by the European Association for Cardio-Thoracic Surgery (EACTS).Eur.Heart J. 45, 3415–3537 (2024).
CAS一个 Google Scholar一个
Cholesterol Treatment Trialists’ Collaboration.Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials.Lancet 376, 1670–1681 (2010).
Cholesterol Treatment Trialists’ Collaboration.Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials.Lancet 385, 1397–1405 (2015).
Bohula, E. A. et al.Inflammatory and cholesterol risk in the FOURIER trial.循环 138, 131–140 (2018).
CAS一个 Google Scholar一个
Byrne, P. et al.Evaluating the association between low-density lipoprotein cholesterol reduction and relative and absolute effects of statin treatment: a systematic review and meta-analysis.JAMA Intern.医学 182, 474–481 (2022).
CAS一个 Google Scholar一个
Nurmohamed, N. S., Navar, A. M. & Kastelein, J. J. P. New and emerging therapies for reduction of LDL-cholesterol and apolipoprotein B: JACC Focus Seminar 1/4.J. Am.科尔。Cardiol. 77, 1564–1575 (2021).
CAS一个 Google Scholar一个
Pérez de Isla, L. et al.Alirocumab and coronary atherosclerosis in asymptomatic patients with familial hypercholesterolemia: the ARCHITECT study.循环 147, 1436–1443 (2023).
Welty, F. K. et al.Regression of coronary fatty plaque and risk of cardiac events according to blood pressure status: data from a randomized trial of eicosapentaenoic acid and docosahexaenoic acid in patients with coronary artery disease.J. Am.Heart Assoc. 12, e030071 (2023).
CAS一个 Google Scholar一个
Williams, M. C. et al.Artificial intelligence and machine learning for cardiovascular computed tomography (CCT): a white paper of the Society of Cardiovascular Computed Tomography (SCCT).J. Cardiovasc。Comput.Tomogr. 18, 519–532 (2024).
Koetzier, L. R. et al.Deep learning image reconstruction for CT: technical principles and clinical prospects.Radiology 306, e221257 (2023).
Mergen, V., Eberhard, M., Manka, R., Euler, A. & Alkadhi, H. First in-human quantitative plaque characterization with ultra-high resolution coronary photon-counting CT angiography.正面。Cardiovasc.医学 9, 981012 (2022).
Dunning, C. A. S. et al.Classification of high-risk coronary plaques using radiomic analysis of multi-energy photon-counting-detector computed tomography (PCD-CT) images.Proc。SPIE Int.Soc。选择。工程。 12465, 124652T (2023).
Healy, J. et al.Ex-vivo atherosclerotic plaque characterization using spectral photon-counting CT: comparing material quantification to histology.Atherosclerosis 378, 117160 (2023).
CAS一个 Google Scholar一个
致谢
The authors thank the German Research Foundation (DFG) for funding the third Quantitative Cardiovascular Imaging meeting and this Consensus Statement on the quantitative assessment of coronary artery stenosis and atherosclerosis (DE 1361/32-1).This work was also supported by the DFG through its graduate programme on quantitative biomedical imaging (BIOQIC, GRK 2260/1, DFG project number 289347353), the DFG Priority Programme Radiomics (DFG project number 402688427) for the investigation of coronary plaque and coronary flow (DE 1361/19-1: DFG project number 428222922 and DE 1361/20-1: DFG project number 428223139 in SPP 2177/1) and the GUIDE-IT project on data sharing of medical imaging trials (DE 1361/24-1, DFG project number 495697118).
道德声明
竞争利益
M.C.W.has given talks for Canon Medical Systems, GE Healthcare, Novartis and Siemens Healthineers and performed consultancy for Canon Medical Systems and FEops.A.A.G.reports research grant support from GE Healthcare, the Iten-Kohaut Foundation and Promedica Stiftung, has given talks for GE Healthcare and has performed consultancy for Artrya Ltd. J.M.T is supported by the Cambridge BHF Centre of Research Excellence (RE/24/130011) and the Wellcome Trust (211100/Z/18/Z) and has received research grants from AstraZeneca, the British Heart Foundation and General Electric Healthcare.R.V.is supported by institutional research grants from Siemens Healthineers and has received honoraria for lectures/moderatorship from Bayer Healthcare and Siemens Healthineers.I.I.receives institutional research grants from the Dutch Research Council with the participation of Abbott Vascular, Philips Healthcare and Pie Medical Imaging, and institutional research grants from Esaote, Health Holland with participation of Braun and Infraredex, Horizon Europe, the EU Innovative Health Initiative with the participation of Philips Healthcare and Pie Medical Imaging.A.A.-Z.receives grant support from Canon Medical Systems.哈。receives institutional grants from Bayer, Canon, Guerbet and Siemens and receives royalties from Springer Nature for a textbook on cardiac CT.哈。received speaker honoraria from Siemens.R.M.receives speaker fees from Bayer, Bristol Meyers Squib, Philips and Siemens and research grant support from the Swissheart Foundation and the USZ Foundation.E.D.N.is on the Scientific Advisory Board of Caristo and is the immediate Past President of the Society of Cardiovascular Computed Tomography (SCCT; the opinions expressed in this article are the author’s own and do not represent the view of the SCCT).N.S.N.reports grants from the Dutch Heart Foundation (Dekker 03-007-2023-0068), European Atherosclerosis Society (2023), research funding/speaker fees from Cleerly, Daiichi Sankyo and Novartis and is co-founder of Lipid Tools.M.D. was the publications chair of the European Society of Radiology (ESR) from 2022 to 2025 (the opinions expressed in this article are the author’s own and do not represent the view of the ESR).He is also the editor of Cardiac CT (Springer Nature) and has institutional master research agreements with Canon, General Electric, Philips and Siemens, the arrangements of which are managed by Charité — Universitätsmedizin Berlin.He also holds a joint approved patent on dynamic perfusion analysis using fractal analysis (EPO 2022 EP3350773A1 and USPTO 2021 10,991,109).The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiologythanks Meinrad Beer, Leslee Shaw and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
附加信息
Publisher’s noteSpringer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
权利和权限
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s);author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
关于这篇文章
引用本文
Schulze, K., Stantien, AM., Williams, M.C.等。Coronary CT angiography evaluation with artificial intelligence for individualized medical treatment of atherosclerosis: a Consensus Statement from the QCI Study Group.Nat Rev Cardiol(2025).https://doi.org/10.1038/s41569-025-01191-6
公认:
出版:
doi:https://doi.org/10.1038/s41569-025-01191-6