AI helped older adults report accurate blood pressure readings at home
Research Highlights:
- Use of an AI voice agent to prompt self-reported blood pressure readings helped to improve accuracy of blood pressure measures and patient outcomes in a group of majority ages 65 and older patients with high blood pressure.
- The study’s findings demonstrate how integrating AI into care can help to improve home blood pressure monitoring and completion rates, which can lead to improved quality outcomes for patients.
- Note: The study featured in this news release is a research abstract. Abstracts presented at the American Heart Association’s scientific meetings are not peer-reviewed, and the findings are considered preliminary until published as a full manuscript in a peer-reviewed scientific journal.
Embargoed until 10:00 a.m., ET/9:00 a.m. CT, Sunday, Sept. 7, 2025
BALTIMORE, Sept.7, 2025 — Artificial intelligence (AI) voice agents helped older adults with high blood pressure to accurately report their blood pressure readings and improved blood pressure management, according to preliminary research presented at the American Heart Association’s Hypertension Scientific Sessions 2025. The meeting is in Baltimore, September 4-7, 2025, and is the premier scientific exchange focused on recent advances in basic and clinical research on high blood pressure and its relationship to cardiac and kidney disease, stroke, obesity and genetics.
“Controlling blood pressure remains a cornerstone for improving cardiovascular outcomes for patients, however, capturing timely, compliant blood pressure readings remains a challenge, particularly for patients with limited access to care,” said lead study author Tina-Ann Kerr Thompson, M.D., senior vice president of the primary care service line and executive director of the population health collaborative at Emory Healthcare in Atlanta. “In our study, we were able to improve accuracy of blood pressure measures and patient outcomes.”
AI voice agents are conversational systems powered by large language models that can understand and produce natural speech in real time when interacting with humans. This study included 2,000 adults, a majority ages 65 and older, and was designed to evaluate the effectiveness and scalability of a voice-enabled AI agent in engaging patients to self-report accurate blood pressure readings, in place of a phone call with a health care professional about their blood pressure measures. The AI agent also identified patients in need of follow-up medical care based on their blood pressure readings.
The AI voice-agent calls to patients were made using commercially available AI in multiple languages, including English and Spanish. A blood pressure reading outside the threshold range for readings that vary based on the presence of other conditions, such as diabetes, resulted in the call being escalated to a licensed nurse or medical assistant. The presence of symptoms such as dizziness, blurred vision or chest pain also prompted escalation of the call. Escalation to additional care was immediate in urgent situations or within 24 hours for non-urgent issues.
The patients were contacted by the voice agent to provide recent blood pressure readings or to conduct live measurements during the call. After the call, the readings were entered into the patient’s electronic health record and reviewed by a clinician. Call routing and referrals for care management were prompted for patients with difficult-to-control high blood pressure. This process reduced the manual workload by clinicians and resulted in an 88.7% lower cost-per-reading. This amount was calculated by comparing the cost of commercially available AI voice agents with the use of human nurses to perform similar tasks that result in successfully obtaining patient self-reported blood pressure readings.
The study found that integrating AI into clinical workflows lowered costs and improved care management for patients. During the study period:
- 85% of patients were successfully reached by the voice-based AI agent.
- Of those patients, 67% completed the call, and 60% took a compliant blood pressure reading during the call. Among these patients, 68% met CBP (controlling blood pressure) Stars compliance thresholds.
- Overall, 1,939 CBP gaps were closed, elevating the measure from 1-Star to 4-Star performance—a 17% improvement. The Medicare Advantage (MA) and Healthcare Effectiveness Data and Information Set (HEDIS) CBP measure increased from a previously reported 1-star rating to 4-star rating.
- At the end of each completed call, patients received a two-question survey to rate their satisfaction on a scale of 1 to 10, with 10 being 100% satisfied. Among the completed calls, the average patient-reported satisfaction rate exceeded 9 out of 10, reflecting an excellent overall experience with the voice-based AI agent.
“We were surprised by the high patient satisfaction scores after interacting with artificial intelligence-based voice agents,” said Thompson. “We are excited for what that means for the future, since patient engagement and satisfaction are so critical to health care outcomes.”
“This could be a game-changing study,” said Eugene Yang, M.D., M.S., FACC, an American Heart Association volunteer expert. “Accurate blood pressure readings are essential to improving control, and new approaches can help make that possible. Breakthrough AI technologies like this could transform how we manage blood pressure by reaching patients wherever they are and addressing critical barriers, such as limited access to care and gaps in patient support.” Yang, who was not involved in this study, is a professor in the division of cardiology and the Carl and Renée Behnke Endowed Chair for Asian Health at University of Washington School of Medicine.
The study has several limitations. This study was observational and did not have a control group. The consecutive AI calls were not compared to human calls; instead, AI voice-calls were deployed because it was not possible to make an adequate number of human-only calls. In addition, the study was retrospective, meaning it reviewed existing data, and evaluation was completed after the clinically identified calls were already made.
Study details, background and design:
- Participants included 2,000 adults; a majority were ages 65 or older (average age of 72 years; 61% women) receiving care for high blood pressure.
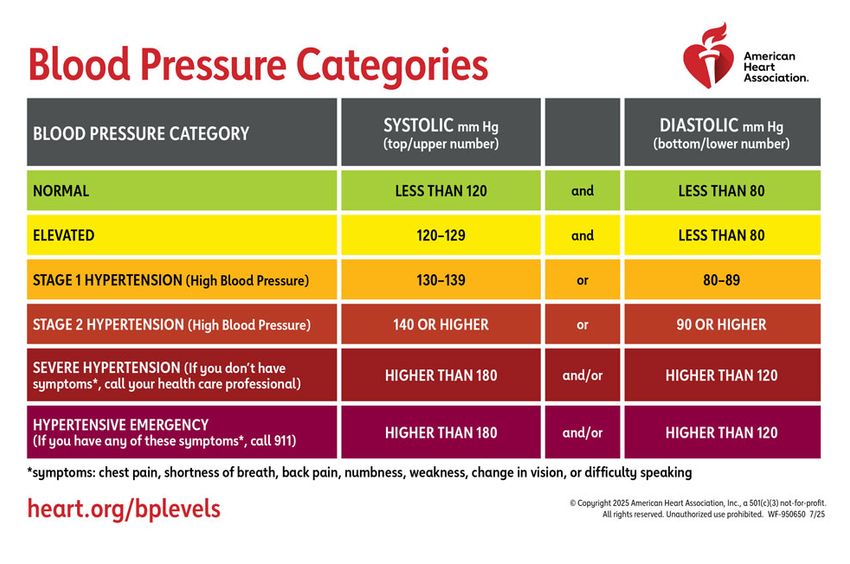
- Review of electronic health records identified patients who were missing blood pressure data or whose most recent BP reading was not within the normal range of <120/80 mm Hg. Patients with these gaps in data were tagged to receive calls from the AI voice agent.
- The study was conducted with patients at Emory Healthcare in Atlanta during a 10-week period. Patients received at least one phone call during the study. Patients received more than one call if they did not answer the phone.
- Patients with open gaps in managing blood pressure were identified through electronic medical records (EMR) and payer analytics. Patient lists were reviewed to ensure the information in their records was correct, and they were verified for outreach by a clinical operations team to ensure real-time accuracy of gaps before outreach to the patients.
- AI texts, phone calls from the conventional care team, recent clinical visits where documentation could be found for a blood pressure reading and generative AI voice agents were used to contact patients to provide recent blood pressure readings or take their blood pressure reading during the call. These included any recent clinical visits where documentation could be found for a BP recorded.
- A post-call validation step was integrated into the workflow, in which readings were entered into the EHR, reviewed by a clinician and submitted as supplemental data to close the Stars quality gap. For patients with uncontrolled high blood pressure, clinical escalation referrals were made to care management teams.
- The Centers for Medicare and Medicaid Services (CMS) developed the Star Ratings system, known as MA Stars, to rate Medicare Advantage (MA) (Part C) and prescription drug (Part D) plans on a 5-star scale with 1 being the lowest score and 5 being the highest score. MA plans are plans from private insurance companies approved by Medicare and not issued by Medicare itself. Hospitals, care centers and clinicians are eligible to receive a bonus payment increase if they achieve at least a 4-star rating.
Self-measured blood pressure is a focus area of Target:BP, an American Heart Association initiative that helps health care organizations improve blood pressure control rates through an evidence-based program. Home blood pressure monitoring is recommended for all adults with any level of high blood pressure, as noted in the Association’s new 2025 guideline on high blood pressure, released last month.
Note: Oral presentation #107 is at 10:00 a.m. ET, Sunday, Sept. 7, 2025.
Co-authors, their disclosures and funding sources are listed in the abstract.
Statements and conclusions of studies that are presented at the American Heart Association’s scientific meetings are solely those of the study authors and do not necessarily reflect the Association’s policy or position. The Association makes no representation or guarantee as to their accuracy or reliability. Abstracts presented at the Association’s scientific meetings are not peer-reviewed, rather, they are curated by independent review panels and are considered based on the potential to add to the diversity of scientific issues and views discussed at the meeting. The findings are considered preliminary until published as a full manuscript in a peer-reviewed scientific journal.
The Association receives more than 85% of its revenue from sources other than corporations. These sources include contributions from individuals, foundations and estates, as well as investment earnings and revenue from the sale of our educational materials. Corporations (including pharmaceutical, device manufacturers and other companies) also make donations to the Association. The Association has strict policies to prevent any donations from influencing its science content and policy positions. Overall financial information is available here.
Additional Resources:
- Available multimedia is on right column of the release link.
- American Heart Association news release: Urgent need to develop best practices to advance use of AI in cardiovascular care (February 2024
- American Heart Association news release: New high blood pressure guideline emphasizes prevention, early treatment to reduce CVD risk (August 2025)
- American Heart Association health information: What is High Blood Pressure?
- American Heart Association health information: How to Accurately Measure Blood Pressure at Home
- American Heart Association health information: The Facts About High Blood Pressure
- Follow AHA/ASA news from the meeting on X @HeartNews #Hypertension25
###
The American Heart Association’s Hypertension Scientific Sessions 2025 is a premier scientific conference dedicated to recent advancements in both basic and clinical research related to high blood pressure and its connections to cardiac and kidney diseases, stroke, obesity and genetics. The primary aim of the meeting is to bring together interdisciplinary researchers from around the globe and facilitate engagement with leading experts in the field of hypertension. Attendees will have the opportunity to discover the latest research findings and build lasting relationships with researchers and clinicians across various disciplines and career stages. Follow the conference on X using the hashtag #Hypertension25.
About the American Heart Association
The American Heart Association is a relentless force for a world of longer, healthier lives. Dedicated to ensuring equitable health in all communities, the organization has been a leading source of health information for more than one hundred years. Supported by more than 35 million volunteers globally, we fund groundbreaking research, advocate for the public’s health, and provide critical resources to save and improve lives affected by cardiovascular disease and stroke. By driving breakthroughs and implementing proven solutions in science, policy, and care, we work tirelessly to advance health and transform lives every day. Connect with us on heart.org, Facebook, X or by calling 1-800-AHA-USA1.
For Media Inquiries and AHA Expert Perspective:
AHA Communications & Media Relations in Dallas: 214-706-1173; ahacommunications@heart.org
Michelle Kirkwood: Michelle.Kirkwood@heart.org
For Public Inquiries: 1-800-AHA-USA1 (242-8721)
heart.org and stroke.org
